© Turkuvaz Haberleşme ve Yayıncılık 2024
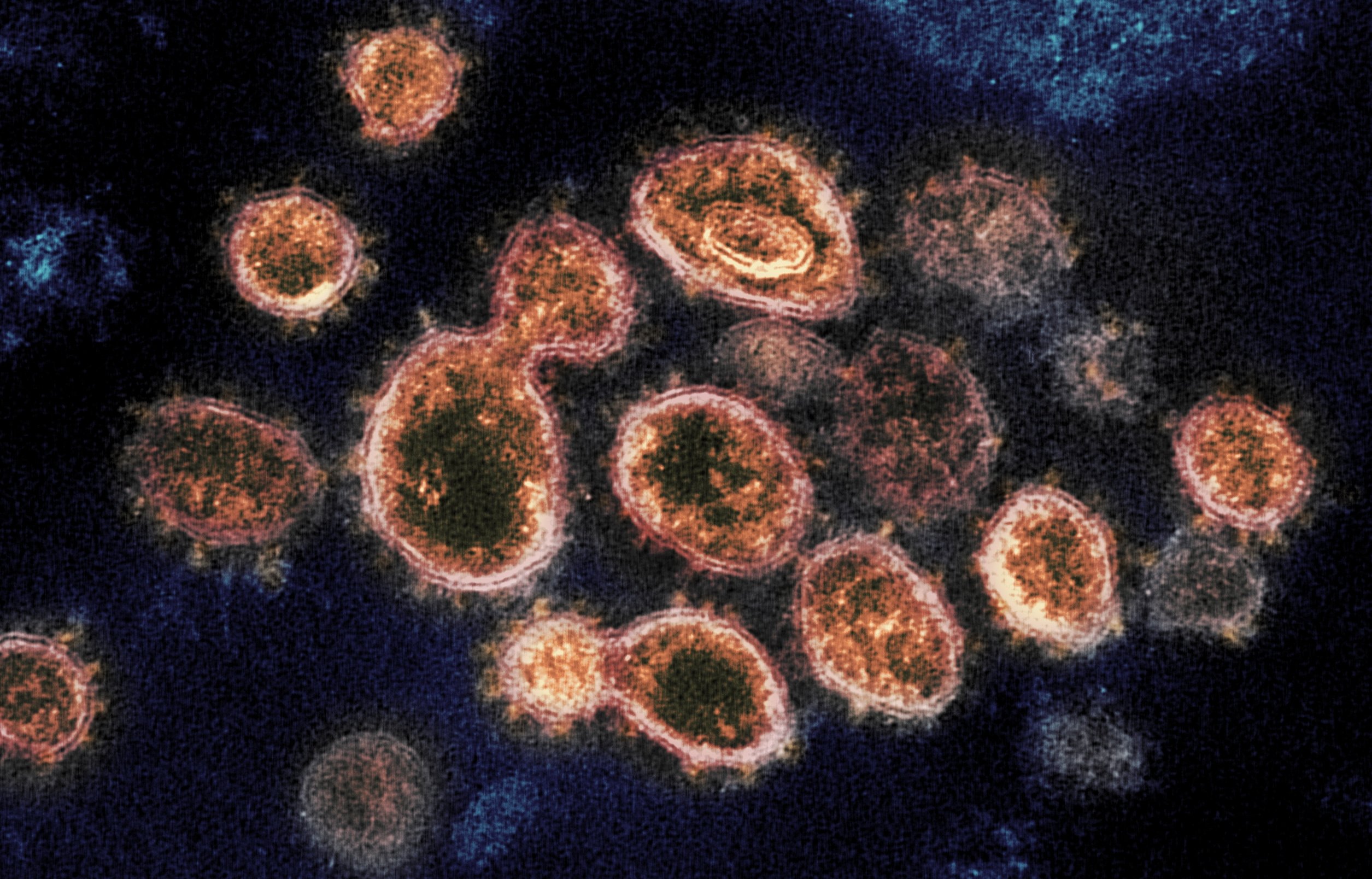
This week's brief roundup of some of the latest scientific studies on the novel coronavirus and efforts to find treatments and vaccines for COVID-19 focuses on how the virus spreads, including by whom and for how long patients stay infectious, while long-term complications experienced by hospitalized cases could be worse than previously thought.
COVID-19 patients likely not infectious beyond 9 days
COVID-19 patients are unlikely to spread infectious virus particles beyond nine days after symptoms begin, even though the virus is detectable in the nose and throat and stool for much longer, according to data compiled by U.K. researchers from 79 studies.
RNA, the genetic material of the virus, was detectable in throat swabs for an average of 17 days from symptom onset and for up to 83 days. But RNA itself is not infectious, lead researchers Müge Çevik and Antonia Ho told Reuters in an email. PCR tests that diagnose COVID-19 are so sensitive they can also detect non-viable genetic material, they explained.
Studies that attempted to culture infectious virus were not successful beyond day nine, the researchers reported on medRxiv ahead of peer review. "Many studies agree patients with SARS-CoV-2 infection have a very high viral load ... in the first week of illness (and) seem to be most infectious from symptom onset to day five," Çevik and Ho said.
"This suggests many people by the time they are tested are already beyond their most infectious period," so those who suspect they may be ill should isolate themselves right away. People without symptoms are also likely most contagious soon after becoming infected, they said.
Survivors of severe COVID-19 face nerve, muscle problems
Doctors expect that people with severe COVID-19 who survive weeks on a ventilator will face a well-documented condition called ICU-Acquired Weakness. The condition leaves long-term intensive care unit (ICU) patients with nerve degeneration, muscle wasting and debilitating weakness.
Doctors at one large U.K. hospital say a significant proportion of their ICU patients with COVID-19 also develop a nerve condition called "axonal mononeuritis multiplex" with severe pain, loss of sensation and movement problems confined to isolated regions on their limbs. Of 69 patients with severe COVID-19 who were discharged from the ICU after spending an average of a month on mechanical ventilators, 11 (16%) had axonal mononeuritis multiplex.
While nerve damage is well recognized as an occasional complication of intensive care, "our experience suggests that such deficits are common and frequently disabling in patients recovering from COVID-19," they wrote in a paper posted mid-July on medRxiv ahead of peer review.
"Given that this complication is evident in a significant proportion of the patients ... the rehabilitation burden globally could be substantial," they said.
Beware of reach of coronavirus 'superspreaders'
People with COVID-19 are unlikely to transmit the virus via exhaled droplets unless they are "superspreaders," researchers said in JAMA Network Open at the end of July. But because there is no way for the average person to identify a superspreader, everyone should wear masks, they said.
Researchers looked at data on the viral load in sputum and swab samples from coronavirus patients and available information on patterns of microdroplets exhaled and coughed by healthy individuals. They calculated that in a closed room about the size of a small office, most infected people would not put many viruses into the air. But a person with a high viral load could put out a substantial amount of infectious material when simply breathing normally, they said.
Emissions can be further boosted if such individuals are coughing, singing or shouting and more so when combining those activities with physical exercise, Michael Riediker of the Swiss Centre for Occupational and Environmental Health told Reuters.
Emissions from a coughing superspreader even in well-ventilated rooms can result in airborne concentrations that bring along a serious risk of infection, he added.
New T-cell data may point way to longer-lasting vaccines
Researchers who examined immune cells from 35 New Jersey patients recovering from COVID-19 have discovered that 90% of their foreign invader-killing T cells aim for targets other than the spike protein on the surface of the virus – the current focus of many vaccines in development.
This suggests that "second-generation vaccines will need to incorporate these targets to generate long-term immunity to COVID-19," Gavin MacBeath of TScan Therapeutics told Reuters. Killer T cells, also known as cytotoxic or CD8+ T cells, clear viral infections and appear necessary for long-term immunity to coronaviruses, he explained.
His team also found that "patients' CD8+ T cells recognize the same, relatively small number of targets that are unique to the novel coronavirus and don't tend to mutate, paving the way for diagnostic tests that detect immunity based on T cells," MacBeath said. The findings were reported in July on medRxiv ahead of peer review.