© Turkuvaz Haberleşme ve Yayıncılık 2025
The global race for the coronavirus vaccine seems to be coming to a pivotal end. Several pharmaceuticals are announcing critical breakthroughs and orders have started to pile up. The United States and Europe have either secured or preordered vaccines from mostly Pfizer and BioNTech, Moderna or Oxford-AstraZeneca along with several others still in development, with the number of doses requested for mass inoculation surpassing billions.
Turkey, along with Brazil, Chile and Indonesia, has opted for the CoronaVac vaccine, developed by the China-based biopharmaceutical company Sinovac Biotech. Turkey's order of 50 million doses will soon be secured and at least 25 million people are expected to be vaccinated by the end of February. Volunteer health care workers have already begun taking part in Phase 3 trials.
But how does this vaccine as well as the others for COVID-19 work and how will the process continue going forward? Let's take a look.
How do vaccines work?
When a virus enters the human body, the immune system produces antibodies in response. If you remember the French animated series "Once Upon a Time... Life" (or "Micro Patrol" as some know it), you can consider these Y-shaped proteins the body's soldiers who defend against all threats.
When the body is exposed to a new virus it needs time to train these soldiers to specialize in fighting against that particular virus. Vaccines speed up this process by helping the body's immune system get familiar with the virus beforehand to prepare for when it comes into contact with the real thing. Either by introducing an inactive or weakened virus into the body or a part of the virus's protein, vaccines, in essence, provide antibodies with the blueprint or game strategy of their viral enemy.
In short, a vaccine mimics viral infection but not so well that we fall really ill.
FEARS AND MISCONCEPTIONS
Why don't we have a cure for COVID-19 instead of vaccines?
To create a true "cure" scientists have to stop viral replication, aka stop the virus from making copies of itself. There are drugs that serve this process such as chemotherapy agents. But because the photocopying mechanism inside our bodies are our cells, any drugs created to halt this would be greatly toxic to them. Creating targeted treatment would not only take years, but it would also bring about a lot of side effects.
So, why don't we have vaccines for Ebola or HIV?
Actually, there are several vaccines for Ebola, but they are mainly used to control outbreaks, not for widespread prevention. The first one to receive approval from the U.S. Food and Drug Administration (FDA) was rVSV-ZEBOV in December 2019, with studies indicating a 95%-100% effectiveness rate.
The case with HIV (human immunodeficiency virus) is more complex, though. To date, only two people have been cured of AIDS, the disease caused by HIV, which has happened via bone marrow transplants from people who are genetically resistant to HIV. Although rare, there are such people in the world. However, this method of curing is not viable nor cheap or easy. Hence, lifelong medication is still the norm. There isn't yet a vaccine for HIV because no healthy human or immune system has been able to naturally defeat the virus on its own. And as vaccines are based on mimicking the natural response our immune system gives to fight the virus, this has proven impossible for HIV, even after over 40 years of research. When it comes to HIV, the fact that it attacks T cells, our body's defenders, makes it difficult as our defense system shuts down.
Are coronavirus vaccines different from other vaccines?
Coronavirus vaccines are mostly developed using the same methods as traditional vaccines, though there are some new techniques. Currently, the three main methods are inactivated virus vaccines, live attenuated virus vaccines and the newly developed messenger RNA (mRNA) method.
Inactivated virus vaccines use pathogens that have been grown in culture. These pathogens are then killed and lose the capacity to produce diseases. However, as they retain the blueprints of the virus's working mechanism, they can help the immune system recognize the virus and prepare for battle. This method is used for several diseases including hepatitis A, rabies and most commonly for flu shots. Because the virus is dead, several doses over time or booster shots can be needed.
Live attenuated or weakened virus vaccines contain a small part of a weakened and mostly harmless but still viable (live) virus. They create a stronger and longer-lasting immune response which can sometimes offer lifetime protection. Live virus vaccines need to be kept cool to protect their viability, so travel is not a good option for them. Vaccines for measles, chicken pox, yellow fever and many others are produced with this method. Not all people are suitable candidates for these vaccines, namely pregnancy and being on immunosuppressive medication such as medicines for cancer or autoimmune disorders are contraindicated.
The mRNA method is a new development in vaccination studies. They don't use weakened or inactivated viruses, they instead use a part of the virus's genome to instruct the cells to produce a certain kind of protein which in response triggers the immune system to produce antibodies, aka soldiers. While these soldiers fight the foreign proteins, they also learn how to protect the body against the virus. Although this is a relatively new method, it has been researched extensively over the last couple of decades. Manufacturing this type of vaccine is much more timesaving and potentially safer, but they require extremely low temperatures for storage and transport.
TLDR (Too Long; Didn't Read): In summary, the inactivated viruses (used in vaccines) are the dead body of an enemy general and the murder weapon; there is information to be gained, but it can be limited. Live attenuated viruses are alive but a drunk enemy general. They share a lot more information, but there is a slight chance they may spill their drink all over you. Lastly, the mRNA vaccines are like an allied general, warning and instructing you against the enemy.
Will the vaccine change my DNA?
If someone is trying to instill fear in you by saying the vaccine will change you by splicing your DNA, they are fearmongering. It is true that viruses can't replicate independently in the body and hence need to latch onto a human cell. For the coronavirus to do this, it needs its spike proteins to bind to the ACE2 proteins in our cells.
If you think of cells as protein-making factories, the DNA would be management or the headquarters. These factories get instructions to produce necessary proteins from the DNA, which are written down on RNA. These instructions are carried out via machines in the factory. The virus is the spy or hacker trying to get into the factory to change these instructions. If it can bind to the cell, then it can tell the system to make its own proteins and duplicates. So, the virus doesn't even get inside the nucleus to come anywhere near the DNA.
Another misconception that people have is that with the mRNA method, they believe the body will start making new viruses inside of their bodies because they are introducing a part of it. If you were to compare natural infection and this type of vaccine, you'd see that with the former, your body is made to deal with the invader.
With natural infection, the virus unloads all of the new instructions into your cells, whereas with mRNA you only get a part of it – the part on how to make spike protein. If you do not have all the instructions to create something new and complex, you will fail. Hence, your body won't be able to make the virus, it will just learn how to create an antibody to stop spike proteins from attaching themselves to the ACE2 proteins on your cells.

A WORD ON THE NEW UK STRAIN
What is this new mutation in the UK and should I be worried?
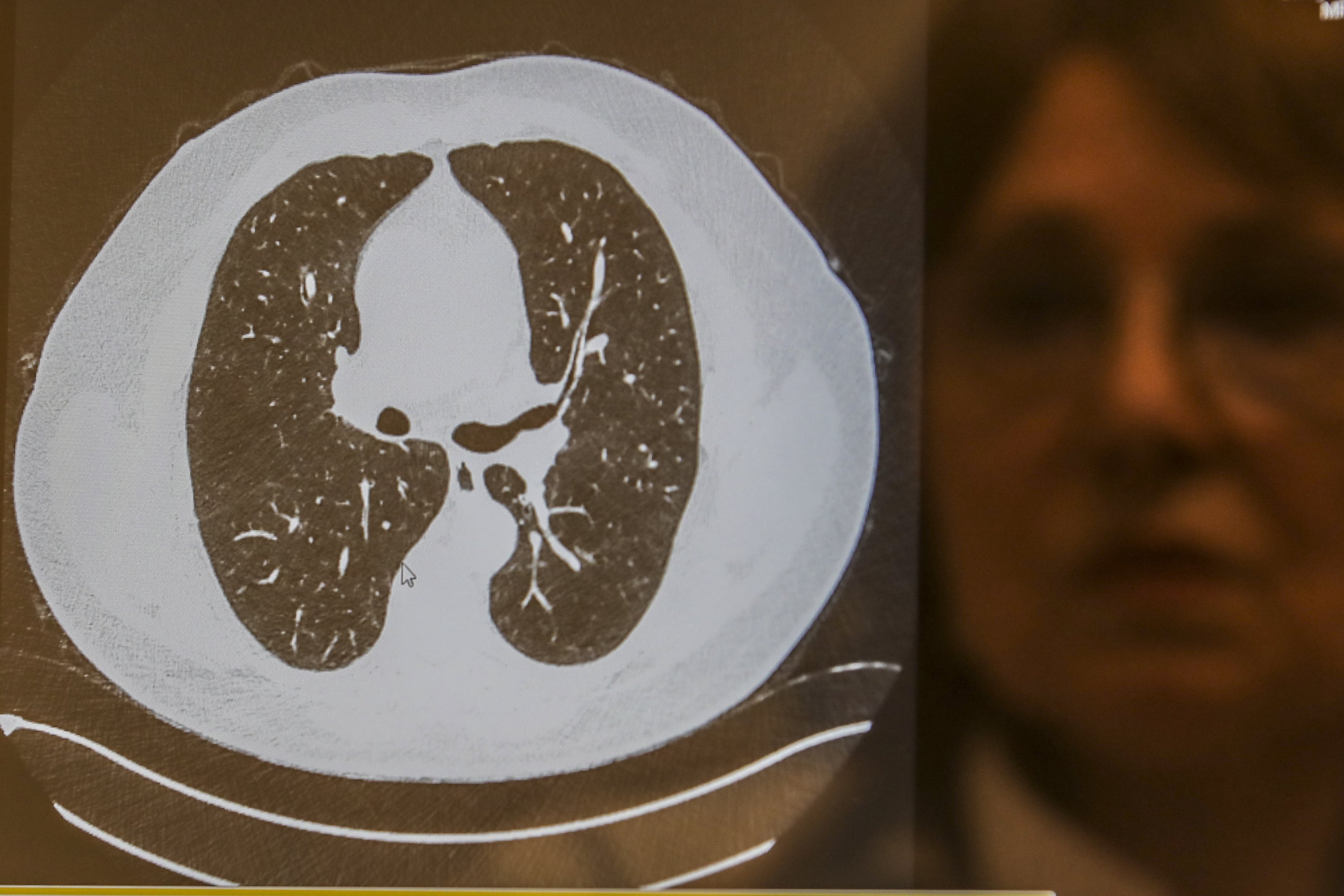
Mutations happen naturally in viruses over time and mostly they don’t cause more severe diseases. The influenza virus, for example, mutates almost every year. The mutation detected in the coronavirus is also not thought to affect the severity of the virus, only its infection rate and capability. This means that the new mutated strain needs fewer particles to make people sick and is more communicable so will spread wider easier.
Viruses use different methods to bind to cells. The coronavirus uses proteins called the spike protein. The new variant of the virus, currently called VUI-202012/01 (Variant Under Investigation, year 2020, month 12, variant 01), is the result of a combination of 14 mutations, according to a report by Public Health England. The most significant of these is the N501Y mutation in the spike protein that the virus uses to bind with ACE2 receptors.
The recent increase in cases in and around the London area is now believed to be caused by this change. It is estimated that as a result of the mutation, the transmissibility of coronavirus is increased around %70. The mutation does not mean the virus is more dangerous, just more infectious.
Does this render current vaccines useless?
Mutations present in the new variant affect the spike protein that most vaccines target. However, a single change in the protein is highly unlikely to make the vaccines obsolete, reports the British Medical Journal. Most of the scientific community agrees that vaccines, which target many regions of the spike protein, will retain their efficacy.
Uğur Şahin, CEO at BioNTech who is partnering with Pfizer on the vaccine, said that he was confident that the vaccine will maintain its efficacy despite the mutation. Statements from the World Health Organization (WHO) and the European Medicines Agency (EMA) have echoed Şahin’s sentiments and cautioned against panic.
COMPARING OPTIONS
How is CoronaVac different from other coronavirus vaccines?
The CoronaVac vaccine, developed and produced by Sinovac, uses the inactivated virus technique. It contains inactivated or rather killed viral particles. When injected into the body these particles set off the alarms of the immune system, so it attacks the intruders. In doing so the vaccine teaches the immune system how to respond to the live virus without risking a serious disease response.
Meanwhile, the vaccines developed by Moderna and Pfizer use the mRNA method. AstraZeneca's coronavirus vaccine, on the other hand, was developed with a technique similar to live attenuated virus vaccines and contains a virus based on a modified chimpanzee adenovirus altered to look a lot more like the coronavirus.
CoronaVac's method is a more traditional and a successful one, said Luo Dahai, associate professor at the Nanyang Technological University. The method employs a traditionally developed method used for vaccines such as the rabies vaccine, based on years of research history. On the other hand, newer methods although thoroughly researched, don't yet have precedence for large-scale use.
"MRNA vaccines are a new type of vaccine and there is (currently) no successful example (of them) being used in the population," Dahai pointed out to the BBC; yet this doesn't mean they are not brilliant breakthroughs for science and medicine.
One of the main advantages of CoronaVac, and similarly Astrazeneca's, is that it can be stored in standard refrigeration units, between 2 and 8 degrees Celsius (35 to 46 degrees Fahrenheit). Meanwhile, Moderna's vaccine has to be stored at minus 20 degrees Celsius while Pfizer's vaccine needs to be kept at minus 70 degrees Celsius.
How do the efficacy rates of vaccines compare?
The efficacy of various vaccines was a big question for some time. With some of the vaccines completing their Phase 3 trials, reports are finally emerging on the effectiveness of them. There are many still in Phase 2 and 3.
Pfizer-BioNTech's vaccine is reported to have a 95% efficacy based on late-stage trials. Initial results from Moderna's vaccine were described as particularly impressive and its efficacy rate is reported as 94.5%. AstraZeneca has not yet revealed data regarding its trials and reports a range between 70% and 90%, an acceptable rate for wide use.
CoronaVac is still in the later stages of its Phase 3 clinical trials, which are ongoing in Turkey, Indonesia and Brazil. The progress has been described as very promising. In Indonesia, 97% of trial participants produced antibodies. Its final efficacy rate is yet to be announced.
In comparison to the other vaccines, CoronaVac has managed to produce a quicker immune response in trials and it has already received the green light for emergency use in high-risk groups in China.
Professor Luo Dahai recently told the BBC that the preliminary data points to it being an effective vaccine with confirmation on its efficacy rate to be gained after Phase 3 trials are completed.
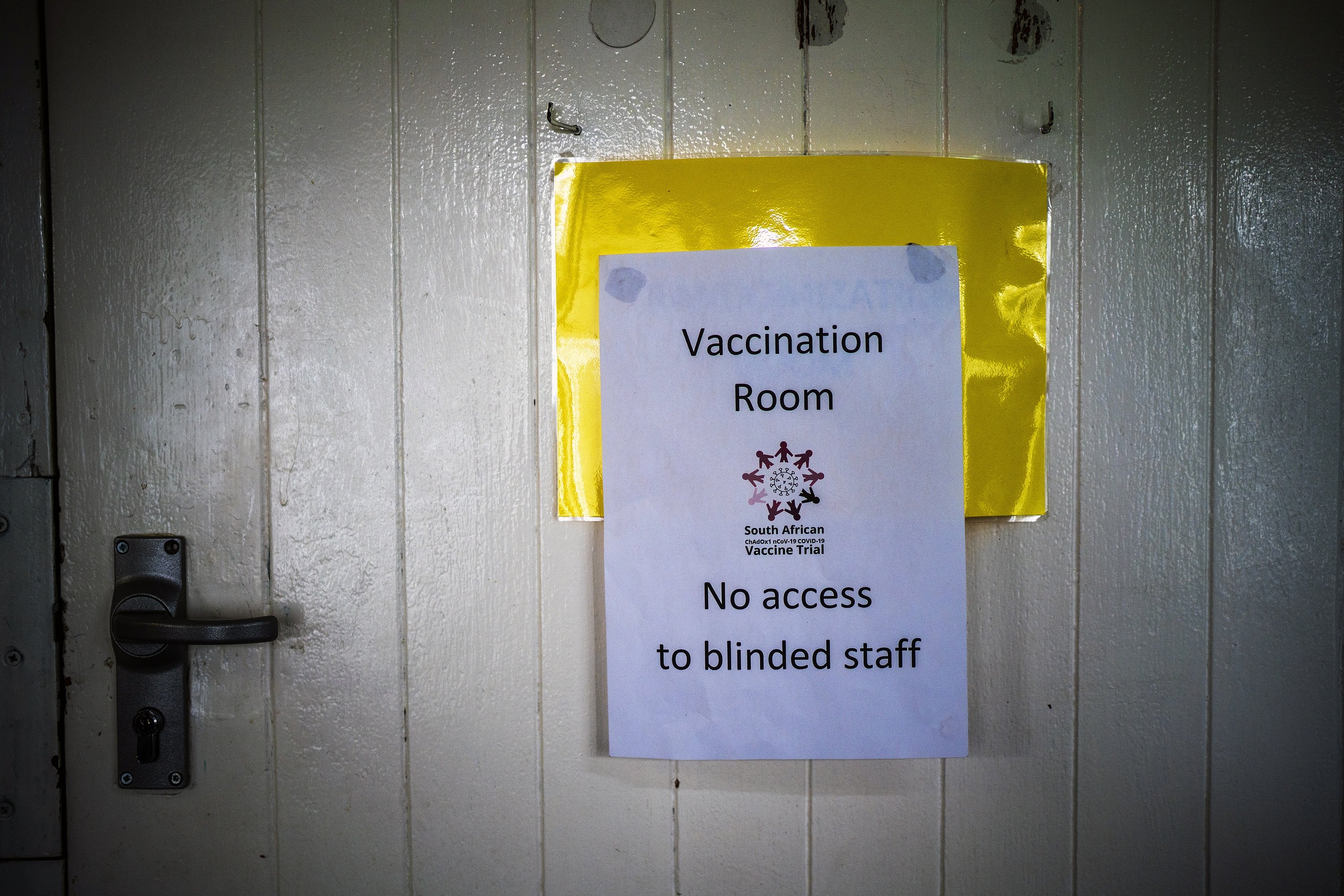
"These trials are randomized, observer-blind, placebo-controlled ... with thousands of participants. This is the only way to prove a vaccine is safe and effective to be used at the population level," explained Dahai.
MORE HESITANCIES
How safe are the vaccines and why were scientists so quick?
The fact that the measles, mumps, and rubella (MMR) vaccine is the fastest ever approved and took four years to develop and license has raised many questions for the new coronavirus vaccines. The MMR vaccine, like the new COVID-19 vaccines, have been based on prior research, dating back to World War II and before, which shortens the timeframe. The COVID-19 pandemic is a deadly disaster on a global scale, which gives scientists plenty of motivation to speed things up and return to "normal." A misconception that people have is that research for a COVID-19 vaccine started only when the pandemic began. However, the basis of the research was established long ago, first in the severe acute respiratory syndrome (SARS) outbreak in 2002 and then subsequently with the Middle East respiratory syndrome (MERS) outbreak in 2012. All of these viruses that cause these diseases are from the coronavirus family.
All vaccines undergo a rigorous testing process, which includes pre-clinical analysis, research and tests on cells, and safety trials on animals before they even begin testing on humans. After a vaccine passes successfully through these stages, clinical trials begin in humans, divided into three phases. Only after completing all of these three phases with a clean bill of health and without serious side effects can it receive the green light on public use.
Although the global pandemic has shaken the pharmaceutical industry and put it under immense pressure to achieve a working, successful coronavirus vaccine, that doesn't mean safety is thrown out the window. Considering that these are all stages that biopharmaceuticals go through without the promise of any customers, the fact that millions of preorders have been placed for a vaccine not yet on the market gives these companies great motivation.
A coronavirus vaccine goes through the same process of testing, clinical trials and phases as every other vaccine. The only difference in the process is the length of these stages, their timing and their production numbers. Instead of taking six months to find volunteers or waiting a year for sufficient funding, as the whole world has funneled limitless funds into finding a treatment or cure for COVID-19, money or people have not been a concern. In addition, trials have commenced shortly after the other one starts and have "overlapped," therefore eliminating waiting times. No safety regulations or protocols have been disregarded and all developments have been checked and verified by independent sources.
Even after all three phases of human trials end, it will be up to the discretion of countries' own health ministries and medical systems to whether they employ them for mass use or not.
What about allergies?
There is no evidence to suggest that any of the ingredients used for the vaccines could cause harm and so far, there have been no health risks reported for CoronaVac or the vaccines from Pfizer and Moderna. Most vaccines have their active ingredient, which is the virus or a piece of it, and then the rest is basically filler and stabilizers. Fats (lipids) act as a layer of protection for the main ingredient, while salts (e.g. sodium chloride) and sugar (sucrose) are used to stabilize the pH or the concoction during freezing.
Pfizer's vaccine has produced some allergic reactions in very few people, which scientists say could be because of the fats or polyethylene glycol, or PEG. But PEG is a petroleum-based compound widely used in cosmetics and food, as well as a laxative in much higher doses. AstraZeneca's work in Brazil was also briefly halted when a participant committed suicide, but the trials continued once an investigation found the death was unrelated to the vaccine and the participant was on a placebo. Two British volunteers also suffered allergic reactions and both had a history of severe reactions, but it was quickly solved with a shot of epinephrine.
Currently, only people with a history of significant allergic reactions (to vaccines or other medications that lead to anaphylactic shock) are recommended to wait for further reports as a precaution.
The chances of having an allergic reaction to the ingredients inside vaccines are very rare, about one in a million. Such reactions surface quite quickly, and that's why doctors observe patients for about 30 minutes before discharging them to intervene if necessary.
Why do I need two doses?
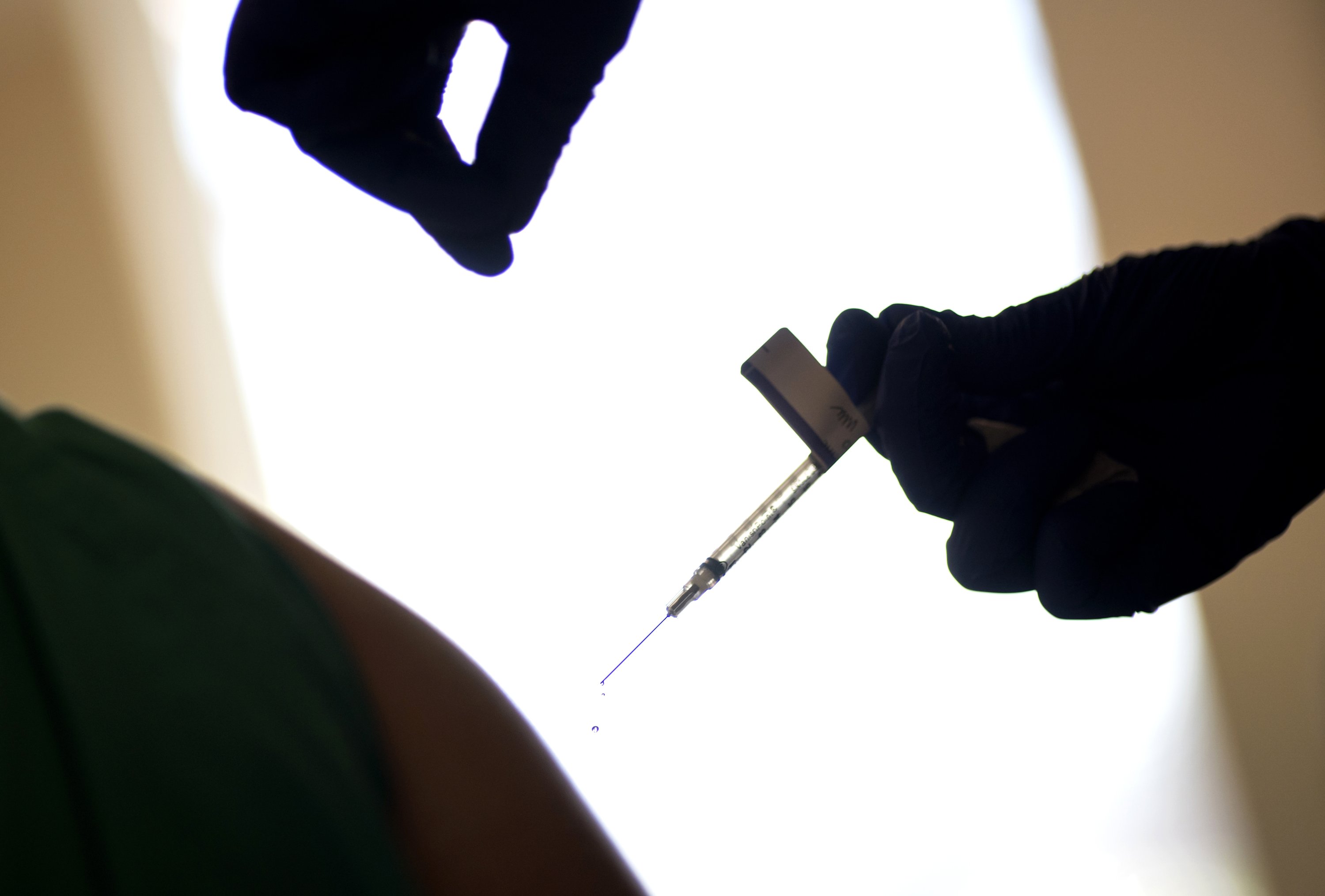
Vaccines, especially inactivated virus vaccines, may require more than one dose to provide the necessary protection. So far most of the coronavirus vaccines including Pfizer-BioNtech's, Moderna's and Oxford-AstraZeneca's need two doses, with one being a booster. Similarly, CoronaVac also requires two injections with a 14-day interval.
Two doses are needed because the first one primes the immune system to get it familiar with the virus. However, as it has been observed in natural infection cases as well, the antibody concentration in our bodies wanes over time, which means we start losing immunity. Antibody production typically goes down after the two-week mark, which is when a booster shot will be administered to keep antibody levels in the body steady. The second shot is, hence, called a booster and helps the body generate memory B and T cells to remember its prior enemy and fight it off.
Do recovered patients need to get vaccinated too?
Normally if a person gets ill and successfully recovers, the body will produce antibodies on its own to fight off the virus the next time it encounters it. However, in the case of COVID-19, immunity has been ever-changing, with some recovered patients losing immunity in as little as three months. Antibodies are also known to rapidly decline after infection. Whether or not these people will receive a vaccine will likely be up to whether they have produced SARS-CoV-2 antibodies or not, and what health officials advise.
However, most doctors have recommended survivors get a vaccine even if they have natural protective immunity as the degree of protection is still unknown. They also think getting vaccinated may even enhance immunity from initial infections.
When will I be immune after getting my shot?
Immunity has been a contested topic, with those infected having natural immunity for anywhere from three months to eight months or more. However, scientists have found that the concentration of antibodies in the bloodstream falls rapidly after infection. This is attributed to the fact that the virus can modulate the immune system to stop the body from maintaining memory B and T cells to remember how to fight this enemy.
Fourteen to 21 days after getting your shot is when scientists say you will gain immunity, which is when levels of immunoglobulin G (IgG), a type of antibody, goes up in your body. People who have taken part in vaccine trials have also been immune for at least 120 days and it is still ongoing. In light of the rate of antibodies they are producing, scientists project up to two years of immunity with a vaccine.
TURKEY'S ROADMAP
How will the vaccination process be handled?
After shipment of the doses, countries will first begin their own tests. In Turkey, the Ministry of Health is closely monitoring the process. When the vaccines arrive in Turkey, they will be subject to examination and the state-run Turkish Medicines and Medical Devices Agency (TITCK) will assess their efficacy.
Subsequently, early/emergency use authorization will be granted if Turkish labs confirm the shots are safe. The following process will unfold in four stages. First, health care workers will be vaccinated alongside citizens older than 65 with priority given to people living in care homes or those disabled.
The second stage will include essential workers and people over the age of 50 with at least one chronic illness. The third group will be people under the age of 50. Young adults and workers will not be covered in the first two stages. The fourth and final group will consist of the rest of the population not included in the first three groups.
Nearly 60 million people are expected to be vaccinated by June 2021. The vaccines will mainly be administered in health care institutions and clinics, but workplace physicians in big companies and factories will also be able to vaccinate on site after training. The vaccines will also be provided to people with disabilities at home.
How much will the vaccine cost?
Health Minister Fahrettin Koca said the vaccines would be provided free of charge, reaffirming President Recep Tayyip Erdoğan's earlier remarks that a deal was agreed for 50 million doses and that Turkish citizens would not be charged for their vaccination.
What does the future hold?
Although vaccines will provide a major boost in the struggle against the coronavirus, scientists urge people to temper their expectations. A long journey awaits before people can resume their normal daily lives, with masks and social distancing practices expected to be in place for a long time. Vaccination will take time both on the production side and the implementation side. For the time being, wear a mask, practice good hygiene, abide by social distancing rules and you can remain cautiously optimistic for 2021.
