© Turkuvaz Haberleşme ve Yayıncılık 2025
Breast cancer is one of the most common types of cancer in women and in Turkey, one out of every four women diagnosed with cancer suffers from breast cancer, according to the Breast Health Association (MEMEDER).
Early diagnosis and treatment continue to prove crucial in saving lives, which means regular checkups and screenings should be widely adopted. In addition to regular self-examination of breast tissue to check for lumps, bumps and other irregularities on and around the breast, including the armpit, medical examinations by a doctor or thorough checks with equipment could help nip cancer in the bud.
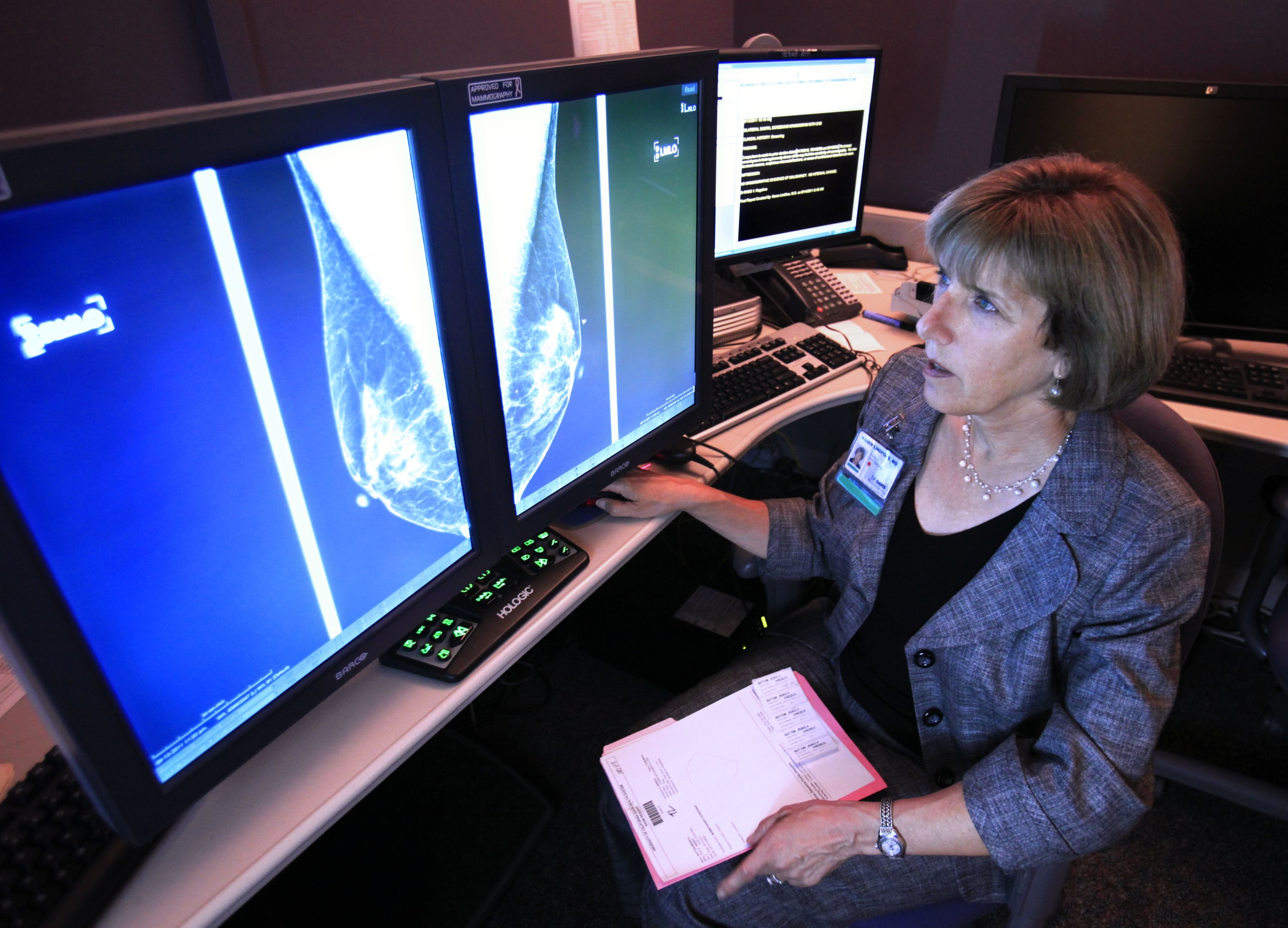
The most reliable method of early detection by far is mammograms, which is an X-ray of the breast that looks for changes and signs that might point to breast cancer. A mammography machine compresses the breast between two plates to get an image. Most women report feeling only slight discomfort during the X-ray process from the pressure against their breasts. The procedure lasts a few minutes and only very few women experience extreme pain, most cases with a tumor. Newer machines have both reduced the amount of compression and duration, making the experience more comfortable.
Meanwhile, ultrasonography uses high-frequency sound waves to examine the breast and converts them to an image, without radiation. It is a painless procedure, but those with tender lumps may experience some pain.
However, the rate of women going in for mammograms is very low, considering the prevalence of breast cancer in Turkey. According to Eurostat, only 36% of Turkish women went in for an annual mammogram in 2019, while this rate in Finland was 83% in 2018.
So, on the occasion of Breast Cancer Awareness Month, here are some of the most frequently asked questions about mammograms and ultrasounds and answers by radiology specialist Muhittin Mümtaz Özarar.
Q: Can you get a mammogram while breastfeeding?
The density of breast tissue increases in breastfeeding women. The main reason for this is the milk secretion in the lactating breast and the subsequent filling of milk ducts as well as the increase in the density of gland tissue that produces milk. This can slightly reduce the sensitivity and accuracy of mammographies. However, it does not completely render results from the procedure invalid as it still assists in the diagnosis. While less dense tissue such as fat shows up gray on the breast X-ray, denser tissue will appear white. This could create confusion as tumors are also made up of dense tissue and hence look white on the image. But medical professionals will always order more tests if something looks suspicious.
Doctors also advise mothers to breastfeed before having a mammogram to reduce the amount of milk present in the breast tissue, thus reducing the density to provide a clearer image.
Q: Can women with breast implants have a mammogram?
Breast implants do not constitute an obstacle for the examination of breast tissue via mammography, ultrasonography or MRI. The pressure applied during a mammogram will not damage the implant, contrary to popular belief.
Detailed images can be obtained by selecting the correct dose and program for examining the breast. However, those with implants are advised to get an ultrasound as well as a mammogram during their annual breast exam.
Q: Is there any harm in having a mammography and does it increase cancer risk?
Because mammograms use X-rays many are concerned that the radiation could contribute to cancer, despite, theoretically, the chance of radiation from such diagnostic machines triggering cancerous cells in the body being very low. Especially nowadays, thanks to advancements in modern technology, such procedures emit very little radiation. To put things into perspective, the amount of radiation you get from a single mammogram is the same as the amount you are subjected to on a flight.

Q: What should you do before going for a mammography?
There is no need to prepare before a mammogram. The only thing you should make sure is not to use cosmetics such as ointments on your skin or powdered deodorants on your underarms before getting screened. These products can show up as white spots on the X-ray and be labeled suspicious. Also, it might be beneficial for women who experience a lot of breast sensitivity before and during menstruation to have the screening done after for more ease and comfort.
Q: Who might need a breast ultrasound?
Breast ultrasonography is performed as a complementary examination in patients with dense breast tissue, those who have undergone a mammography for screening or diagnostic purposes, as a primary procedure in the evaluation of the axillary region (ie. underarms) for those under 40 years of age and as a guiding method in biopsy procedures.
Breast ultrasounds are not usually done to screen for breast cancer. They do not require special preparation either and can be carried out even during pregnancy.
Q: Should women over 40 have breast ultrasounds or mammograms? Can breast ultrasounds be performed in over 50-year-olds?
From the age of 40, regardless of family history, mammograms should be done routinely every year for screening. Ultrasounds should be performed complementary to mammography, especially in those with dense breast tissue, decreased mammographic sensitivity and suspicious findings during a mammogram. Ultrasonography can be performed easily at any age.
Q: How often should you have a mammogram?
Mammographies should be done regularly once a year from the age of 40 onward. The examinations can be recommended at an earlier age for women in high-risk groups, ie. those with a family history of breast cancer. Consult your doctor for the best frequency.
Q: How often should you be examined if you have a family history of breast cancer? Are mammographies sufficient on their own in high-risk cases?
People with breast cancer in their family should have a mammogram and ultrasound once a year starting at the age of 40. If a first-degree relative was diagnosed with breast cancer under the age of 40, then doctors recommend starting screening for cancer 10 years before cancerous growth was detected in said family member. If your relative was diagnosed at age 35 then you should be going regularly for checkups starting at age 25.
In addition to an annual mammogram and ultrasound, doctors also recommend routine MRI follow-ups for women in the high-risk group.
